A Letter from Dr. Lisa Charbonneau, Encompass Health Chief Medical Officer

Healthcare is complicated. At Encompass Health, we understand that and want to make it a little less complicated. In this guide we want to equip you with the information and tools you need to make the best decisions for your health as you or a loved one ages. While the title of this guide addresses those 60 and older, it is really designed for anyone who wants to take control of their healthcare.
Yes, healthcare can be complicated, and it tends to get more complicated as you age, but a little knowledge and some advanced planning can go a long way in navigating you or a loved one’s care in your 60s and beyond.
Cutting through the Medical Jargon: How to Talk to Your Doctor
Sometimes, interpreting a doctor’s medical jargon can feel like trying to understand a foreign language.
Most patients and families, don’t want to admit they don’t understand when a doctor begins explaining a complicated illness or condition, and instead sit quietly nodding in affirmation.
Jargon is pervasive in all professions, but it has its greatest impact when doctors try to communicate with patients. People’s lives are at stake. Healthcare professionals have their own verbal shorthand that may be highly effective when they speak to each other but causes confusion when used with laymen.
The use of jargon begins in medical school. A medical student can quickly rattle off that, “Mrs. Jones had a syncopal episode last night without any evidence of arrhythmia. I don’t think it was vagal but I ordered a 2D echo and holter. I still can’t rule out a vertebrobasilar event.” Everyone wearing a white coat understands this secret language, but as a patient lying in the bed, you may feel terrified and confused.
Medical Jargon is Everywhere
The average American reads and speaks at an eighth- or ninth-grade level, yet doctors assume that their patients will understand their obscure communication.
Multiple studies have looked at the use of jargon by doctors and the failure of patients to understand them. One study of 249 emergency room patients reported
that 79% did not know that the word hemorrhage was the same as bleeding and 78% did not know that a fracture was a broken bone. In case you think these were illiterate, underprivileged people, 45% of the people in the study were college educated. We cannot assume that the lawyer or English professor has any more understanding than someone with less education.
What Can You Do to Interpret the Medical Speak?
There are some steps that you and your families can take so you don’t fall into the same trap that so many do. One simple program is the “Ask Me 3” program that provides you with three questions to ask your doctor.
- What is my main problem?
- What do I need to do?
- Why is it important for me to do this?
Unfortunately, you may still get jargon-packed answers. So, here are a few more tips to make sure you walk away with a clear understanding of your problems.
- If you do not understand what your doctor is saying, immediately stop them and ask them to use simpler language. Don’t pretend that you understand when you do not.
- Tell the doctor what you think they said to be certain that you understood them. This is called a “teach back.”
- If you feel you need more time, ask to schedule another visit in the near future. This may be a telehealth visit and you will have the opportunity to have others listen in and help you.
- If the doctor is busy, ask if there is a nurse or assistant who can answer your questions.
- Take a trusted friend with you for another set of ears and even to take notes.
- Ask who you can call if you still have questions when you get home.
Understanding Medicare

If you or a loved one are nearing the Medicare age but are unsure what this benefit provides or the plan that is best for you, we are here to help you understand your options. Medicare is the national insurance program for adults age 65 and older. It’s also a benefit most working adults pay for throughout their lifetime.
Throughout the years, Medicare has evolved and extended the amount of plans available. Understand your options now, so you can pick the best plan for you or your loved one when the time comes.
What to Consider When Picking a Plan
When it comes to deciding between a traditional Medicare plan and a Medicare Advantage plan, consider two things: your income and your freedom to choose your provider. As you add supplemental plans to traditional Medicare, it can cost more than Medicare Advantage plans. However, with traditional plans, you have the freedom to choose any Medicare-approved, certified provider anywhere. Most Medicare Advantage plans require you to see a provider within their network and may require prior approval or a referral for certain procedures or healthcare services
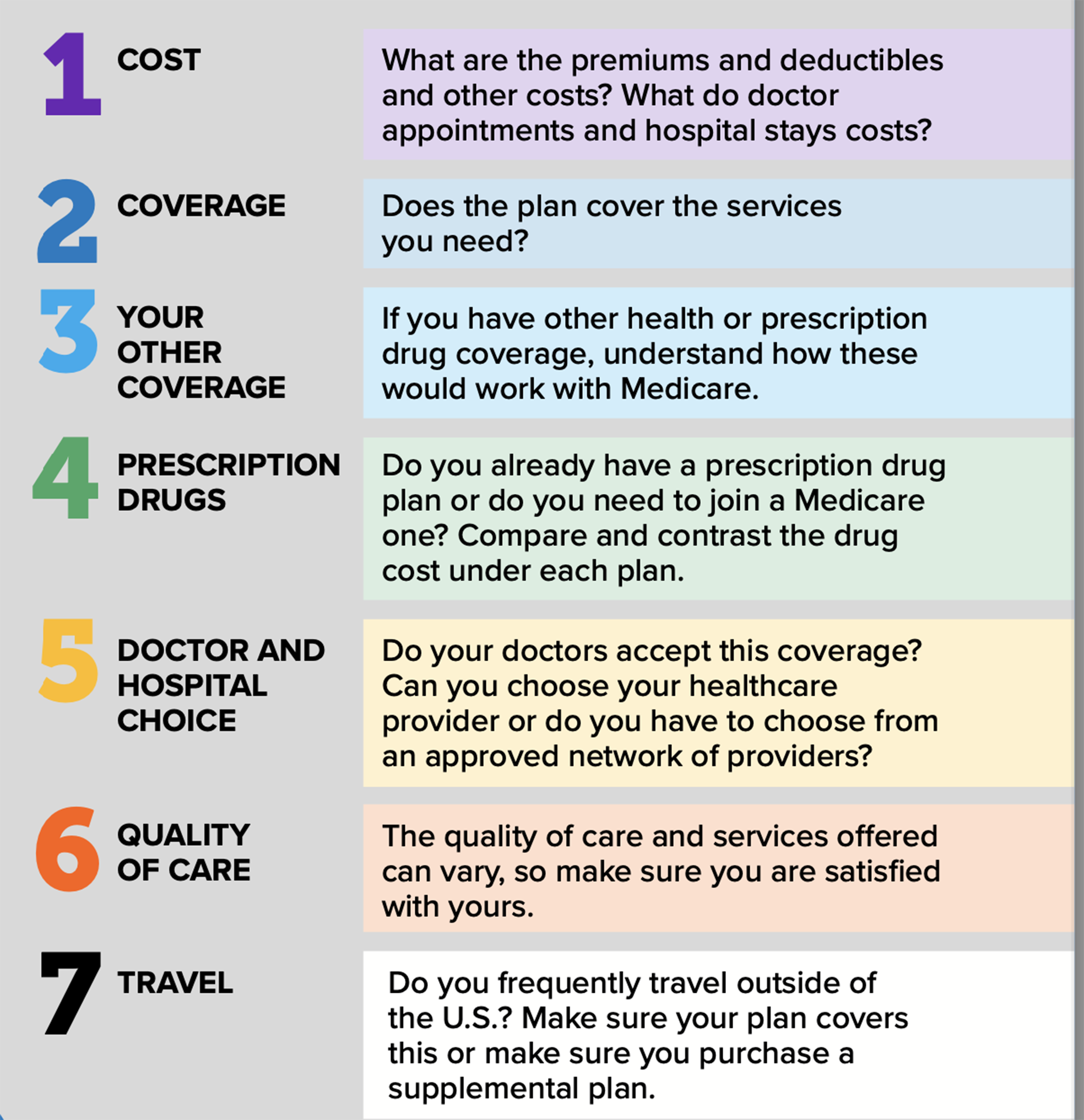
If you’re still searching for answers on what the best plan is for you, Medicare offers these seven things to consider when selecting your Medicare coverage.
How Do You Enroll?
You are automatically signed up for Medicare at age 65. However, if you want to select a Medicare health or drug plan, you have a seven-month period around your 65th birthday to sign up for one. This is called the initial enrollment period, and it:
- Starts three months before you turn 65; if a plan is selected during this period, it will go into effect the first day of the month you turn 65.
- Includes the month you turn 65; if a plan is selected during this period, it will go into effect the first day of the month following your 65th birthday.
- Ends three months after you turn 65; if a plan is selected during this period, it will go into effect the first day of the month after you enroll.
If you later decide to change your plan or join a plan after that seven-month period has closed, enrollment is open each year from Oct. 15 to Dec. 7. Changes or enrollment during this time period will go into effect the following January.
What are the Different Plans?
In general, there are two types of Medicare plans: traditional Medicare and Medicare Advantage.
- Traditional Medicare includes Parts A and B. Part A is automatic and includes hospital insurance, which covers hospital stays, as well as skilled nursing facilities and hospice. Part B is optional and is deducted from your Social Security should you enroll. It includes medical insurance, which covers outpatient services, as well as some physician visits and preventative care. Other supplemental plans can be added through private insurance companies; these are paid for out-of-pocket.
- Also referred to as Medicare Part C or MA plans, Medicare Advantage is an all-inclusive plan that includes both parts A and B, as well other coverage such as prescription drugs, dental and more, depending on the plan. These plans are offered through private Medicare-approved companies. If you join a Medicare Advantage plan, you will likely be required to choose healthcare providers that participate in your plan’s network.
There are a variety of Medicare plans out there today, so as you near the Medicare age of 65, start researching your options to find the one that best meets your needs.
You Have a Choice in Your Care—Know Your Options
During a medical emergency, there might not be time to determine your options for care, but once that emergency is stabilized, your physician or case manager could recommend you transition to another care setting as part of your recovery. These settings—known as post-acute care—include home health, inpatient rehabilitation, skilled nursing homes and long-term acute care hospitals.
Your care team could refer you to one of these settings based on your abilities and goals, but as a patient, you have a choice in selecting which facility you go to. In fact, it is your right as a patient. The Center for Medicare/Medicaid Services refers to this as patient choice.
What is Patient Choice
In 2019, the Center for Medicare/Medicaid Services updated its discharge planning rules to require providers to inform you of your choices when it comes to your post-acute care options. Compare providers near you with this tool from Medicare.gov.
Your referring clinicians—typically a physician and/or a case manager—are required to inform you of the different care settings available in your area that are appropriate for the level of care you require. They also have to tell you if they or their organization have any financial ties to those listed and to share information from those providers, so you can make an educated choice.
The information they share should be related to your recovery goals. Depending on the setting of care, some of that information could include data surrounding rehospitalization (the need to transfer back to the acute care hospital) and patient satisfaction scores, as well as return to community rates.
While all this information can be empowering, it can also be overwhelming, especially if you are not familiar with the different settings of post-acute care.
What are the Different Settings of Care and Which is Best for You

As defined by the Medicare Payment Advisory Commission, post-acute care is rehabilitation or palliative care that a patient receives after a stay in an acute care hospital, or in some instances, in lieu of a hospital stay. That care can take place in the home or in a facility, depending on the patient’s needs. Medicare recognizes four primary types of post-acute care:
- Home health is care that is provided in the home to help you recover after an illness or injury. Your doctor or other provider can refer you to home health and work with you and the agency to determine how many visits you are eligible to receive each week. Home health is designed to meet you where you are. If you’re recovering from a surgery or a recent hospital stay or managing a disease or injury, home health provides care in the comfort of home. Home health services include nursing, therapy, nursing aides and social workers.
- Inpatient rehabilitation hospitals provide a hospital level of care with intensive therapy to help you regain your independence and ultimately return to your community after an illness or injury. While at an inpatient rehabilitation hospital, you will receive three hours of therapy a day, five days week. You will also have frequent visits from a rehabilitation physician and other physicians, depending on your needs. Nursing careis provided around the clock, and a multi-disciplinary team that includes rehabilitation physicians, nurses, therapists, dietitians, pharmacists and case managers will design a unique care plan to fit your goals. Conditions commonly treated at rehabilitation hospitals include stroke, head or spinal cord injuries, neurological disorders such as Parkinson’s and multiple sclerosis, amputation and hip fractures.
- At a skilled nursing facility, you will receive therapy and nursing care. However, unlike inpatient rehabilitation facilities, there are no legal requirements mandating the number of hours of care per day that must be provided. Physician visits are not as frequent, either.
- If you or your loved one has had a particularly extended and medically complex hospital stay, a long-term care hospital may be recommended. At a long-term care hospital, you will receive nursing and rehabilitation care for an extended period of time. Many patients referred for this level of care are not yet able to participate actively in rehabilitation and may require assistance breathing.
Will Insurance Cover My Care?
That depends on your insurance and your coverage. You do have to meet certain medical requirements for the different settings of care to receive Medicare coverage. Also, some Medicare plans, such as Medicare Advantage ones, limit you to providers within their network. Work with your care team or primary care physician to determine if you meet the requirements of a particular setting. Make sure to discuss your goals, so they can fully understand your long-term needs and the setting that will best help you meet them. In some circumstances, you can consult with your preferred provider to see if they can work with your insurance to help you receive coverage.
Do Your Research
Your care team is required to provide you and your loved one with data regarding the quality of care of providers in your area, but take time to do a little research yourself. Look at patient reviews on websites. Ask family and friends with similar conditions who have had good outcomes and experiences. Where and who you receive care from matters, so take time to look around and find the best provider to help you reach your recovery goals. Perhaps a family member can tour a facility you are considering or take a virtual tour online. By understanding the different settings of care now, you are already taking a step in the right direction.


