Low Impact Exercises
Jul 12, 2021
Email US
Click to Email UsMaintaining our physical health as we age is an important part of overall wellbeing. Making activity part of our daily routine becomes more vital as we age but can also be more difficult.
*Only 35-44% of adults over 75 are physically active.
Seniors should always discuss their physical activity level and ability with their physician. For most, engaging in 30 minutes of moderate activity each day can have numerous long-term benefits.
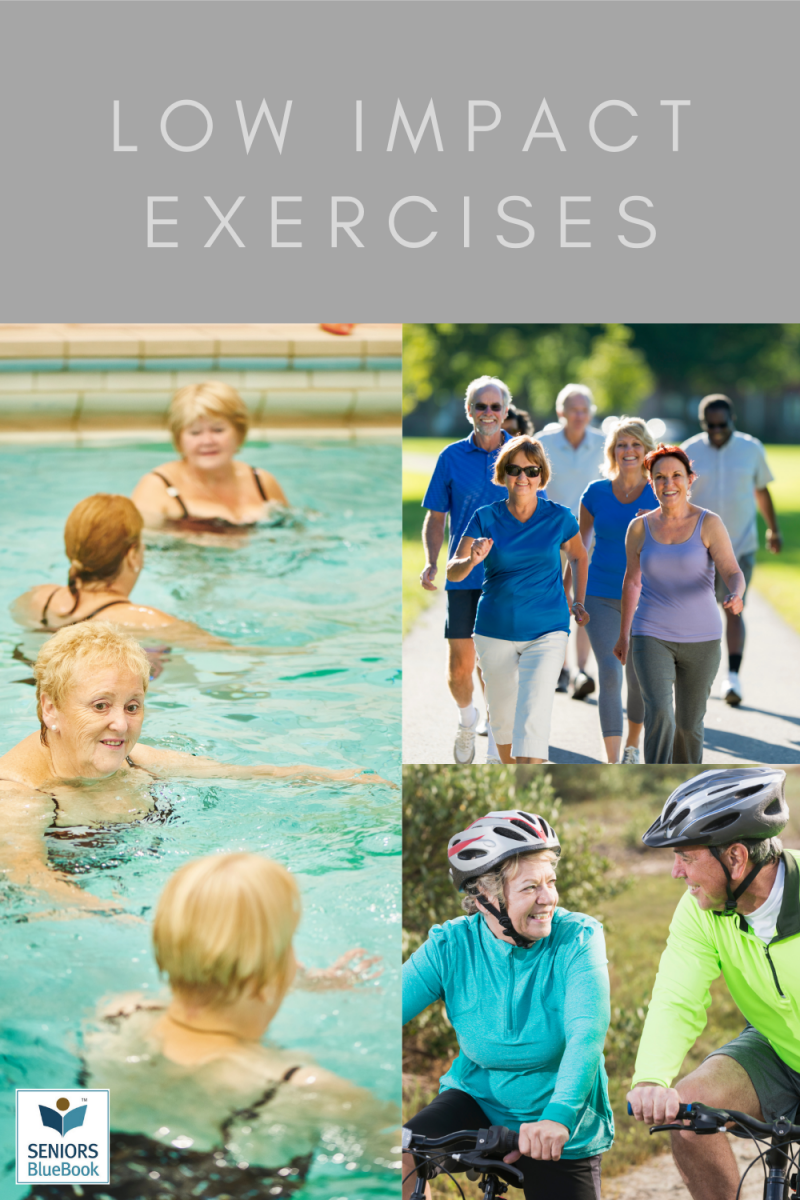
There are a variety of low-impact exercises and activities that can be beneficial for seniors. Low-impact exercise can elevate the heart rate, which in turn has physical health benefits.
While it is typically easier to participate in these less rigorous types of exercise, older adults should always talk to their doctor before starting a new program.
Types of low-impact exercise can include:
Walking: One of the benefits of walking is that, unlike running, its easier on the joints. Plus, it doesnt require any special equipment or a gym membership. With a comfortable pair of tennis shoes and a smooth pathway, someone can start this right away. For the most benefit, keeping a brisk pace for at least 15-20 minutes is important.
Swimming: Whats better than minimal stress on the joints? No stress at all. Swimming provides a number of benefits, including strengthened shoulders and increased lung capacity. Seniors can also take part in water aerobics or walk on underwater treadmills.
Yoga: From improving flexibility and coordination to strengthening your core, theres very little that yoga doesnt do. Additionally, yoga has been shown to improve mood, focus, and overall mental well-being.
Pilates: This exercise allows for very slow and concise movements, designed to improve posture and flexibility. Like yoga, Pilates are known to improve mental well-being.
Cycling:With the proper safety measure in place (including a helmet, shin pads, and appropriate configurations), cycling can do wonders for not only the cardiovascular system but also the joints and various muscle groups.
Weight training: Weight training can be done at home, with small free weights or even moderately heavy objects that you can grip easily, or at a fitness center. Consistent repetition is key, as is advancing to heavier weights over time.
Leg Raises: These can be done at home with no equipment. Simply stand behind a chair, and while holding on to the back of the chair, move one leg to the side and then back. Repeating this, with different variations, can help strengthen lower back and thigh muscles.
Dancing: In recent years, there has been a rise in the popularity of dance class enrollment and for good reason. The constant movement in dancing classes can help circulation and flexibility. Attended these classes can also provide great opportunities to socialize and connect with others.
Comfort Keepers Can Help
At Comfort Keepers, we create individual care plans for every client. These plans include wellness goals that consider physical, mental and emotional health. Our caregivers can help your aging loved one establish a daily routine that promotes a healthy lifestyle. Whether thats taking daily walks or providing transportation to the local gym, well work to provide care that is unique to your loved one. OurComfort Keepersprovide the essentials our clients need to live a healthy, active, and independent life.
To find out more about our other in-home care services, contact us today.
References:
Department of Health & Human Services. Facts and Statistics: Physical Activity. Web. 2017. NIH Senior Health. Exercise: Benefits of Exercise. Web. 2017.
Everyday Health. 10 Surprises About Heart-Healthy Exercise by Beth W. Orenstein. Web. 2014.
American Senior Communities. The Best Low Impact Exercises for Seniors. Web. 2017.
AZ Central. Low Impact Exercises for Seniors by Kathryn Rateliff Barr. Web. 2017.
Other Articles You May Like
A Special Visit: Meals on Wheels America President & CEO Joins Florida Chapter Conference
It was a momentous occasion in Bradenton on May 1, 2025, as we welcomed a very special guest Ellie Hollander, President & CEO of Meals on Wheels America. Her visit was more than ceremonial; it was a heartfelt celebration of community, service, and the vital work being done across Florida to nourish and support our seniors.Ellie flew in from the Washington, D.C. area as the keynote speaker for the Meals on Wheels Florida annual conference, proudly hosted this year by Meals on Wheels PLUS of Manatee. Ellies schedule was packed, but that did not stop her from doing an interview with MySuncoast ABC-7 telling viewers how critical the meal program is to our homebound seniors. Next, Ellie hit the road and delivered meals to some of our senior clients and talked with our volunteers. Ellie also stopped by our Friendship Dining Center program, and participated in a music game the clients love.The Members of the Florida Chapter of Meals on Wheels America named Maribeth Phillips, our President & CEO, as their Board President earlier this year. Maribeth invited Ellie to attend and kickoff the conference. Ellie shared valuable insights with the members in attendance, and her words reenergized the room!The conference included meal providers from across the state, with over 20 different organizations attending. Attendees also heard from Bob Blancato, Executive Director of NANASP, also from Washington, D.C.; Bradenton Police Detective, Jim Curulla on senior scams; Sandra Tapfumaneyi, Chief of Emergency Management Sarasota; Louise Gallagher on Senior Mental Health; and Jennifer Huber from FPL. Chef2Home provided a delicious breakfast and lunch.We are proud to be part of the national network of Meals on Wheels America and grateful to be a part of the state-wide chapter, Meals on Wheels Florida, both working every day to ensure no senior goes hungry.
Help Fight Summer Hunger in Manatee County
As summer approaches, many children in our community are looking forward to sunshine, fun, and time with friends. But for far too many, summer brings something else-hunger.When school cafeterias close for the summer, thousands of local children lose access to the nutritious meals they depend on. Families already struggling to make ends meet are faced with even more pressure. The emotional toll is real. No parent should have to worry if they can feed their child, and no child should go to bed with an empty stomach.At The Food Bank of Manatee, we are stepping up to meet the need. We partner with over 100 local food pantries across Manatee County to reach the families who need us mostbut we cant do it alone.This summer, our goal is to provide: 22,500 meals each week across the 9-week summer break. Thats more than 200,000 meals for children and familiesand every dollar makes a difference.Just $15 provides 10 meals; $30 provides 20 meals; a gift of $150 will provide 100 meals!We know that many in our community want to make a difference. With your support, we can ensure no child goes hungry during the summer months.Please consider making a gift today and sharing this message with others who want to help too. A link to our page is below. A $25,000 Matching Gift to feed children this summer has been offered by an anonymous fund at Manatee Community Foundation. Gifts will be matched $1 for $1 up to $25,000.The Food Bank of Manatee is the only food bank based in our county. We anticipate continued need as families look for nutritional support. Your help matters now more than ever! Please give today!Together, we can bring relief, peace of mind, and full bellies to those who need it most.
Celebrating the Heart of Our Mission: Volunteer Luncheon Honors Our Outstanding Volunteers
On Monday, April 7, 2025, we had the joy and honor of hosting our annual Volunteer Luncheon, a heartfelt celebration dedicated to the incredible individuals who make our mission possible each and every day. Held in a spirit of gratitude and community, the event brought together volunteers with over 100 hours of service for a beautiful luncheon provided by Metz Chef 2 Home. The highlight of the event was the presentation of awards to several outstanding volunteers who have gone above and beyond in their service. From delivering meals with a smile to lending a helping hand wherever needed, these volunteers embody the true spirit of giving.The 2025 award recipients included:Champions Circle: Ten Years of ServiceDan WilhelmChampions Circle: 300+ Hours of ServiceTerri HillChampions Circle: 300+ Hours of ServicePat McDonaldOutstanding Food Bank Volunteer: Terri HillOutstanding Volunteer Ambassador: Veronica Brandon-MillerOutstanding Youth Volunteer: Jonathan MaassenMost Generous Group Ambassador: Lakewood Ranch Elks LodgeOutstanding Volunteer Group: First WatchOutstanding Administrative Volunteer: Barbara BrownOutstanding Friendship Dining Center Volunteer: Pam O ConnorOutstanding Car Loader: Charlie GunnOutstanding Warehouse Volunteer: Lana PaulRookies of the Year: Jeff and Christy MohlerOutstanding Daybreak Adult Day Center Volunteer: Larry BreidenbachOutstanding Telephone Reassurance Volunteer: Reina HuertaVolunteer of the Year: Terri HillTo every volunteer who gives their time and heartthank you. Our Volunteers are the reason we are able to serve our neighbors in need with care, dignity, and hope. We look forward to another year of making a difference together.