Dementia: Improving Communication with Improv | Overview
Kathleen Warshawsky, BSN, RN
For more information about the author, click to view their website: Seniors Blue Book Greater Dallas
Mar 22, 2023
Non-Book Market , Texas - Dallas, Collin, SE Denton & Rockwall Counties
Email US
Click to Email UsDementia: Improving Communication with Improv | Overview is part of a six-part series. Dementia is a degenerative neurological condition that affects millions of people worldwide. As the disease progresses, individuals with dementia may experience difficulties with communication, including problems with memory, language, and understanding. This can make it challenging for caregivers and family members to connect with their loved ones and provide the best possible care. However, there is a promising solution to this challenge: improv. In this six-part series, we will explore how improvisational theater techniques can be used to improve communication and connection with individuals with dementia. By tapping into the power of improv, caregivers can learn how to communicate more effectively, build rapport, and create meaningful experiences with their loved ones.
Dementia is a debilitating condition that affects millions of people around the world. It is a progressive disease that affects memory, thinking, behavior, and the ability to perform daily tasks. As the disease progresses, individuals with dementia may have trouble communicating and may become withdrawn and isolated. However, with the right approach and support, individuals with dementia can still achieve good quality of life.
One approach to supporting individuals with dementia is to meet them where they are at. This means that care providers should strive to understand the individual's unique perspective, experiences, and needs. This approach can help to reduce frustration, confusion, and anxiety and promote a sense of well-being and connectedness.
To meet individuals with dementia where they are at, care providers can use a range of strategies. These may include:
Communication: Communication can be challenging for individuals with dementia. Care providers should use clear and simple language, speak slowly, and allow time for the individual to process information. They should also use non-verbal cues, such as facial expressions and gestures, to convey meaning.
Activities: Activities that are meaningful and engaging can help individuals with dementia to stay connected and maintain a sense of purpose. Care providers should focus on activities that the individual enjoys and are tailored to their abilities and interests.
Environment: The physical environment can have a significant impact on the well-being of individuals with dementia. Care providers should create an environment that is familiar and comfortable, with minimal distractions and noise.
Personalized care: Personalized care can help individuals with dementia to maintain a sense of identity and autonomy. Care providers should take the time to get to know the individual and their preferences and involve them in decision-making as much as possible.
Emotional support: Individuals with dementia may experience a range of emotions, including fear, anxiety, and frustration. Care providers should provide emotional support and validation, acknowledging the individual's feelings and concerns.
Meeting individuals with dementia where they are at requires a holistic and person-centered approach. By understanding the unique needs and experiences of the individual, care providers can support them to maintain a sense of dignity and quality of life, even as the disease progresses.
Communication is a complex process that involves sending and receiving messages, both verbal and nonverbal, between individuals. Effective communication requires the ability to understand and interpret messages, express oneself clearly, and respond appropriately to feedback. For people with dementia, communication can become more challenging as the disease progresses and affects their cognitive and language abilities.
Communication in people with dementia can be impaired due to a variety of factors, including memory loss, difficulty finding the right words, and impaired processing and comprehension of language. This can lead to frustration and anxiety for both the person with dementia and their caregivers. It is important to understand how communication can be affected by dementia and to develop strategies for effective communication.
It is also important to remember that communication is a two-way street, and caregivers and healthcare providers must also be good listeners. Active listening, which involves paying attention to the person with dementia, acknowledging their feelings, and responding appropriately, can help build trust and understanding.
Improved communication with individuals with advanced dementia can lead to several benefits, including better social interaction, reduced feelings of anxiety, and improved quality of life. It can also help caregivers better understand the needs and preferences of the person with dementia, resulting in more personalized care and enhanced well-being for both the caregiver and the person with dementia.
Several studies have explored the benefits of improving communication with individuals with advanced dementia. For example, a systematic review of communication interventions found that these interventions can lead to reduced agitation and aggression among people with dementia, as well as improved quality of life and social engagement (Van't Leven et al., 2013). Another study showed that individualized communication training for caregivers can lead to significant improvements in communication quality and overall well-being for both caregivers and individuals with dementia (Graff et al., 2006).
Moreover, incorporating improvisation techniques, such as mirroring, storytelling, and music, can be particularly beneficial in enhancing communication with individuals with advanced dementia. A randomized controlled trial of music therapy showed that it led to significant improvements in communication and social interaction among individuals with advanced dementia (Raglio et al., 2015). Another study showed that using storytelling and role-playing techniques can lead to significant improvements in communication and emotional well-being among individuals with advanced dementia (Hsu et al., 2018).
Improving communication with individuals with advanced dementia can lead to several benefits for both the person with dementia and their caregiver. Incorporating improvisation techniques can enhance the effectiveness of communication interventions and improve overall well-being.
The components of improv can be applied to dementia care to help improve communication, build trust, and enhance the overall care experience for both the caregiver and the person with dementia.
Components of improv for dementia care include:
Acceptance: Accepting and building on the ideas of others is a key component of improv. In dementia care, acceptance can involve acknowledging and validating the thoughts and feelings of individuals with dementia, even if they are not based in reality. This can help build trust and improve communication.
Listening: Active listening is essential in improv. In dementia care, listening involves paying attention to verbal and nonverbal cues, as well as being open to new ideas and adapting to the needs of the person with dementia.
Agreement: In improv, performers agree to the reality of the scene and build on it. In dementia care, agreement can involve finding common ground with the person with dementia and building on their ideas and interests.
Creativity: Improv is all about creativity and thinking outside the box. In dementia care, creativity can involve finding new ways to communicate, engage, and connect with the person with dementia.
Flexibility: Improv requires performers to be flexible and adapt to changing situations. In dementia care, flexibility can involve being open to new ideas and adjusting communication strategies as needed to accommodate the needs and abilities of the person with dementia.
Playfulness: Improv often involves a playful and lighthearted approach to communication. In dementia care, playfulness can involve using humor and creativity to make communication more enjoyable and engaging for the person with dementia.
Using improv techniques can help caregivers communicate more effectively with individuals with dementia by fostering flexibility, active listening, engagement, and humor. These techniques can help improve the quality of communication and enhance the overall care experience for both the caregiver and the individual with dementia.Improv can help communicate with someone who has dementia by:
Emphasizing flexibility: Improv involves being open and flexible to new ideas and situations. This approach can help caregivers communicate more effectively with individuals with dementia, who may have difficulty following a specific train of thought or conversation. By being flexible and open to new ideas, caregivers can adapt to the needs and abilities of the person with dementia, allowing for more successful communication.
Encouraging active listening: Improv requires active listening and responding to what is being said in the moment. This approach can help caregivers communicate more effectively with individuals with dementia, who may have difficulty following a conversation or articulating their thoughts. By actively listening and responding to the person with dementia, caregivers can help them feel heard and understood.
Fostering a positive and engaging environment: Improv involves creating a positive and engaging environment that encourages participation and creativity. This approach can help caregivers communicate more effectively with individuals with dementia, who may become easily disengaged or frustrated during communication. By creating a positive and engaging environment, caregivers can help individuals with dementia feel more comfortable and open to communication.
Using humor and playfulness: Improv often involves using humor and playfulness to communicate and connect with others. This approach can help caregivers communicate more effectively with individuals with dementia, who may respond well to humor and playfulness. By using humor and playfulness, caregivers can help lighten the mood and make communication more enjoyable and less stressful for everyone involved.
Improv Techniques
There are many improv techniques that can be used on a client with dementia. By incorporating these techniques into their care approach, caregivers can help improve communication, reduce stress, and enhance the overall care experience for the person with dementia.Here are a few examples:
- "Yes, and..." technique: This technique involves building on the ideas of the person with dementia, rather than shutting them down or correcting them. For example, if the person with dementia says, "I want to go to the moon," instead of saying "That's not possible," the caregiver can say "Yes, and maybe we can pretend to go to the moon by looking at pictures of space."
- Mirroring technique: This technique involves mirroring the body language and facial expressions of the person with dementia to help build rapport and understanding. For example, if the person with dementia is smiling, the caregiver can mirror their smile to help create a positive and engaging environment.
- Storytelling technique: This technique involves creating a story with the person with dementia by building on their ideas and interests. For example, the caregiver can start a story with "Once upon a time, there was a cat who loved to play in the garden," and then ask the person with dementia what they think happens next.
- Role-playing technique: This technique involves engaging the person with dementia in role-playing activities to help stimulate their imagination and memory. For example, the caregiver can suggest playing "restaurant" and ask the person with dementia to be the customer, while they act as the waiter.
- Musical improvisation technique: This technique involves using music to engage the person with dementia and create a positive and engaging environment. For example, the caregiver can sing a familiar song and ask the person with dementia to join in or use music to help create a calming environment during a potentially stressful situation.
Using improv techniques in caregiving can greatly enhance the caregiver's relationship with their loved one with dementia. By accepting and validating the individual's experience, caregivers can build trust, improve communication, and increase their loved one's sense of safety and comfort. Improv also allows for creative problem-solving and flexibility, which can be crucial in adapting to the individual's changing needs and abilities. Ultimately, incorporating improv as a form of communication can lead to a more positive, meaningful, and fulfilling relationship between the caregiver and their loved one with dementia.
To Receive Continuing Education Credit for Nursing, Texas Social Work, Texas Licensed Professional Councilor Click HERE.
Read all of the articles in this six-part series on Dementia: Improving Communication with Improv
Dementia: Improving Communication with Improv | Overview
Dementia: Improving Communication with Improv | "Yes and..." Technique
Dementia: Improving Communication with Improv | Mirroring Technique
Dementia: Improving Communication with Improv | Storytelling Technique
Dementia: Improving Communication with Improv | Role-playing Technique
Dementia: Improving Communication with Improv | Musical Improvisation technique
Author: Kathleen Warshawsky, BSN, RN | Publisher Seniors Blue Book Greater Dallas | https://www.linkedin.com/in/kathleenwbsnrn/
To Receive Continuing Education Credit for Nursing, Texas Social Work, Texas Licensed Professional Councilor email Kathleen@SeniorsBlueBook.com for the link.
References:
Alzheimer's Association. (2021). Communication and Alzheimer's. Retrieved from https://www.alz.org/help-support/caregiving/daily-care/communications
Goldsmith, L., & Goldsmith, J. (2019). Communication and dementia. American Family Physician, 99(11), 684-691.
Graff, M. J., Adang, E. M., Vernooij-Dassen, M. J., Dekker, J. H., Jönsson, L., Thijssen, M., ... & Rikkert, M. G. (2006). Community occupational therapy for older patients with dementia and their care givers: cost effectiveness study. BMJ, 333(7580), 1196.
Guzmán, A., & Hegarty, J. (2018). A systematic review of drama therapy interventions for dementia care. Aging & Mental Health, 22(10), 1309-1319.
Hsu, M. H., Flowerdew, R., Parker, M., Fachner, J., & Odell-Miller, H. (2018). A thematic analysis exploring group music psychotherapy for people with dementia in the UK. Journal of Applied Arts & Health, 9(1), 75-87.
Kales, H. C., Gitlin, L. N., & Lyketsos, C. G. (2015). Assessment and management of behavioral and psychological symptoms of dementia. BMJ (Clinical research ed.), 350, h369.
Raglio, A., Bellelli, G., Traficante, D., Gianotti, M., Ubezio, M. C., Villani, D., ... & Stramba-Badiale, M. (2015). Efficacy of music therapy in the treatment of behavioral and psychiatric symptoms of dementia. Alzheimer Disease and Associated Disorders, 29(2), 158-163.
Raglio, A., Gianotti, M., Manzoni, V., Bolis, S., Ubezio, M. C., Villani, D., & Stramba-Badiale, M. (2016). Effects of improvisational music therapy vs enhanced standard care on symptom severity among patients with Alzheimer disease: The IMT-ALZ randomized clinical trial. JAMA Neurology, 73(7), 797-805.
Van't Leven, N., Prick, A. E., Groenewoud, J. G., Roelofs, P. D., de Lange, J., Pot, A. M., & Van't Leven, N. (2013). Communication enhancement between dementia care professionals and dementia patients during daily care. Aging & Mental Health, 17(5), 555-568.
Other Articles You May Like
From Hospital Discharge to Safe Recovery: Western PA Resources Every Family Should Know
From Hospital Discharge to Safe Recovery: Western PA Resources Every Family Should KnowLeaving the hospital is just the first step in recovery. In Western Pennsylvaniawhere seniors often live independently in suburban and rural communitiescareful planning and the right support can dramatically reduce readmissions and help loved ones regain strength at home. Heres a roadmap of essential resources every family should know.Key Transitional Support ServicesTransitioning home safely involves coordinating medical care, home supports, and community resources. Below are five cornerstone programs and agencies that work together to smooth that transition.How These Resources Work TogetherDischarge Planning (UPMC & Other Hospitals)Beginning 12 days before discharge, your hospitals discharge planner will draft a personalized plan covering medications, follow-up appointments, home-safety needs, and recommended home-health services upmc.comupmc.com.Transition Coaching (WPA CCTP)Within 30 days of referral, a coach from the Community Care Transitions Program meets with youeither in-hospital or at hometo ensure youve connected with home-health agencies, durable medical equipment suppliers, and your Area Agency on Aging cms.gov.Home Health & Nursing SupportAgencies like the Visiting Nurses Association provide skilled nursing visits, physical or occupational therapy, and remote monitoring to catch complications earlyreducing emergency calls and readmissions.Medical Advocacy & Ongoing CoordinationIf multiple providers are involved or care plans shift, IKORs RN Patient Advocates help coordinate across specialists, clarify orders, and adjust support levelsso nothing falls through the cracks.Long-Term Supports & Caregiver ResourcesCounty Area Agencies on Aging and organizations like Family Caregiver Alliance offer workshops, respite care grants, home-modification assistance, and peer coachinghelping families sustain safe, dignified care over weeks and months.Tips for a Smooth TransitionBe Proactive: Meet your discharge planner early. Prepare questions about home adaptations, medication side effects, and warning signs.Engage Multiple Resources: Dont rely on a single agencycombine nursing visits, transition coaching, and caregiver education for comprehensive support.Secure Home-Safety Improvements: Ask your Area Agency on Aging about minor repair programs (grab bars, ramps) before discharge.Use 24/7 Support Lines: Keep IKOR or your home-health agency on-call number handy for any urgent medication or care-coordination issues.Plan Follow-Up Appointments Immediately: Schedule primary care and specialist visits within 710 days of discharge to catch early complications.A coordinated, multi-agency approach transforms a potentially risky homecoming into a confident, well-supported recovery journey. If youre planning a hospital discharge for a loved one in Western Pennsylvania, reach out to CarePatrol of Western Pennsylvania for a free consultation. Well help you navigate these programs, arrange tours of post-acute care providers, and ensure a safe, smooth recovery at home.
How to Stay Safe When Living Alone: Practical Tips for Seniors
How to Stay Safe When Living Alone: Practical Tips for SeniorsLiving alone offers independence, freedom, and comfortbut it also comes with unique safety concerns, especially for older adults. Whether you're aging in place by choice or circumstance, taking steps to stay safe can bring peace of mind to you and your loved ones.From fall prevention to emergency planning, here are practical tips for staying safe, secure, and confident while living on your own. 1. Prevent Falls at HomeFalls are one of the most common safety risks for seniors. The good news is that many are preventable with a few simple changes: Remove tripping hazards like throw rugs, loose cords, and clutter. Install grab bars in bathrooms near the toilet and inside the shower or tub. Use non-slip mats in wet areas like the kitchen and bathroom. Ensure good lighting in all rooms, especially hallways and staircases. Wear supportive, non-slip shoes indoors instead of socks or slippers. Keep frequently used items within easy reach to avoid climbing or bending. 2. Invest in a Medical Alert SystemIn an emergency, a medical alert device can be a lifesaver. These systems allow you to call for help with the press of a buttonsome even offer fall detection and GPS tracking. Choose a system that suits your needs (wristband, necklace, or wall-mounted). Look for 24/7 monitoring and an easy-to-use interface. Let family members know how the system works. 3. Stay Connected with Family and FriendsRegular communication not only combats lonelinessit also keeps others aware of your well-being. Set up daily or weekly check-ins with loved ones. Join phone trees or neighborhood watch groups. Use video calls or text messaging to stay in touch more frequently. If you're ever unable to reach out, those regular check-ins could alert someone quickly if somethings wrong. 4. Secure Your HomeHome security helps deter intruders and gives you confidence when living alone. Always lock doors and windows, even when youre home. Install a peephole or video doorbell so you can see whos at the door without opening it. Use motion-sensor lights around entryways. Avoid sharing personal information or travel plans on social media. 5. Create an Emergency PlanBeing prepared gives you control and helps you act quickly if needed. Keep a list of emergency contacts, including family, neighbors, and healthcare providers, in a visible place. Store important medical information (medications, allergies, health conditions) in an accessible location. Plan and practice how to exit your home in case of fire or other emergencies. Keep a flashlight, batteries, and a charged cell phone nearby at all times. 6. Be Cautious with StrangersUnfortunately, seniors living alone can be targets for scams or fraud. Protect yourself by: Never giving personal or financial information over the phone or internet unless you initiated the contact. Being cautious about unsolicited offers, especially for home repairs or investments. Reporting suspicious activity to local authorities or a trusted family member. 7. Manage Medications SafelyMedication mistakes can be serious. Stay organized with: A weekly pill organizer to track doses. Medication reminders via phone alarms or apps. Reviewing medications regularly with your doctor or pharmacist. 8. Consider a Home Safety Assessment Some organizations or healthcare providers offer in-home safety assessments to help you identify potential hazards. They may recommend simple upgrades like handrails, better lighting, or rearranging furniture.At Avondale Care Group of Pennsylvania our services are fully customizable, allowing us to create a care plan that perfectly matches your personal routines and preferences.
Volunteering in Mobile: How Caregivers Can Stay Engaged
Volunteering In Mobile: How Caregivers Can Stay EngagedAccording to a 2023 study, roughly 23 percent of Americans formally volunteer with an organization. Volunteering is voluntary by nature, and theres a reason so many people actively participate in organizations.As a caregiver, you understand the value of helping others. Volunteering comes in many forms and is a wonderful opportunity to help you stay engaged in your community.Benefits Of Volunteering For CaregiversPeople volunteer for different reasons, but many of them start to volunteer because of the personal benefits they can gain. As a caregiver, you may find that caregiving can help you:Recharge: When you volunteer with an organization youre passionate about, your work with them will likely be fun and can help you recharge and take a break from your caregiving dutiesor any other stress in your life.Prevent burnout: Volunteering and focusing on other activities can help prevent caregiver burnout, just as they can help you recharge.Connect with others: Volunteering builds empathy and can help you better connect with people, especially those who come from different backgrounds.Reduce stress: Some volunteer opportunities can be high-stress environments. However, others, such as animal shelters/rescues or gardening/landscaping for community spaces, can be therapeutic and relaxing experiences.Strengthen a sense of purpose and community: When you volunteer for your community, you see first-hand how your work is impacting your immediate surroundings and gives you a sense of purpose.Foster local connections: Volunteer organizations are great places to meet new people, both through the organization and through other volunteers.Local Volunteer OpportunitiesMobile and the surrounding area have many volunteer opportunities to appeal to the interests and skills of all individuals. Whether youre looking to grab free cuddles with a shelter dog or an environmentalist who finds comfort in gardening, youre sure to find something rewarding from one of the volunteer opportunities below.AnimalsIf youre an animal lover who wants an excuse to get face time with all different kinds of pets and animals, consider volunteering with one of these local organizations.Azalea City Cat Coalition: This organization cares for stray cats in Baldwin and Mobile counties. It is regularly looking for volunteers to help with various tasks like trapping and caring for cats, as well as with events.Phillip Cares: This animal welfare organization helps low-income pet owners access food, toys, and veterinary care for their pets. Volunteers with Phillip Cares can help with hosting fundraisers, gathering supplies for homes, and building meaningful connections.Purrfect Partners of Mobile: This non-profit cat and kitten rescue cares for homeless cats and helps them find the perfect forever homes. It is looking for volunteers to assist at the adoption center and foster cat parents.Education And CultureVolunteering can be a wonderful opportunity to learn and feed your curiosity. If you thrive on being a lifelong learner, you may enjoy working with one of these organizations.Goodwill Gulf Coast provides programs and services to families and individuals in need throughout the Gulf Coast. There are plenty of ways volunteers can volunteer here, from small tasks like sorting items to larger initiatives like community outreach and awareness.The National Maritime Museum of the Gulf of Mexico has many immersive exhibits that educate the masses. Volunteers can help greet visitors, assist educators with school groups, and help navigate the exhibit galleries.Big Brothers, Big Sisters is a mentoring organization for Mobiles youth. Volunteers act as mentors and work with their assigned youth members to provide a caring and supportive presence in their lives.The Gulf Coast Exploreum is an educational science center that offers interactive exhibits and hosts events to spark curiosity about science. Volunteers can help with daily operations, special events, and exhibits.EnvironmentIf you love the outdoors and are looking for ways to protect nature, consider working with one of these environmental organizations.Alabama Coastal Foundation works with the public sector and other nonprofits to protect and care for Alabamas coastal environment. Volunteers can assist with cleanup and care initiatives to preserve the Alabama coast.Dog River Clearwater Revival works to provide a safe and clean Dog River Watershed environment. Volunteers can help educate the public and keep the space clean and safe.Caregiving With Visiting AngelsCaregiving can be a demanding job, but its also a rewarding opportunity to assist seniors throughout your communitywhile getting paid to do so! Contact our Mobile office at 251-345-4100 to learn more about caregiving opportunities with Visiting Angels.
Local Services By This Author
STAP (Specialized Telephone Assistive Program)
Hearing/Deaf Products , , Texas,If You Have A Hearing, Vision Or Mobility Problems Accessing Or Using A Telephone - You May Qualify For A Free Telephone! 4 out of 5 Americans over the age of 60 have some hearing, vision or mobility loss. There is help however and it is paid for by you through a government program called STAP, Specialized Telecommunications Assistance Program, by a small charge each month on your telephone bill. Why not take advantage of a benefit youre paying for already? Contact Laura Carr, STAP to learn more about this program and show you what equipment youre eligible to receive FREE OF CHARGE! To qualify, you must be a Texas resident with a problem with vision, hearing or mobility. You are entitled to one FREE phone every 5 years. You can get a cell phone, landline, smartphone or tablet, depending on your disability. Must provide proof of residency. Acceptable forms of residency include:* Texas Drivers License* ID card with address* Voters Registration card* Letter from facility on their stationery* Utility Bill (current - showing address)* Vehicle registration card* Medicaid ID* Medicare Summary This program is for any Texas Resident that has a Vision, Hearing, Mobility- including cognitive problems. They are entitled to FREE telephone equipment (just the device) and they have to pay their monthly charges to their telephone service provider. Depending on their impairment, they may qualifiy for a Landline Telephone with a medical alert system; a Regular Cell Phone (where they can make calls, text, take photos including a medical alert button on the back. If they have a hearing problem, they can receive a 2-way texting device - an Android Smart Phone or Android Tablet. They have to provide their proof of residency for the State of Texas: a current drivers license, Texas ID, Voters Registration Card or a Utility bill showing their name & current address & date. Laura can assist with completing an application, take a photo of their proof of residency - attach to their signed application & send it to STAP headquarters in Austin, Texas. The State processes their application & mails the Voucher for the equipment, directly to the Resident. Once they receive the Voucher, they contact Laura and she will deliver the equipment that is authorized on the voucher to the Resident. NO MONEY CHANGES HANDS. Laura Carr, STAP Specialist has worked with this program for 16 years.Contact Laura at 214-388-0088 or LauraCarr@prodigy.net
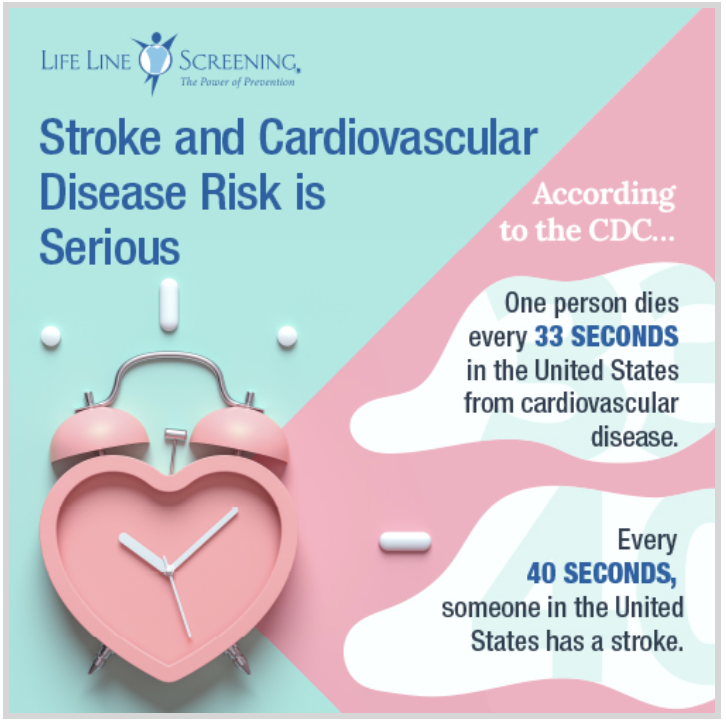
Lifeline Screening
Medical & Wellness , , ,Dont Let a Stroke Ruin Your RetirementYour risk of stroke and cardiovascular disease increases as you age. But the good news is 80% of stroke and cardiovascular disease CAN be prevented.1 If you are age 50 or older, you should be screened.Often there arent any symptoms of a stroke before it occurs, in fact for 4 out of 5 people who have a stroke the first symptom of any illness is the actual stroke.2 But, you can take steps to find out if youre at risk.Life Line Screening is a premier provider of preventive screenings for stroke and cardiovascular disease risk. A simple appointment can identify your risk factors and provide peace of mind or early detection.Screenings are easy, painless, non-invasive and dont require any messy prep work.Life Line Screening has over 14,000 locations across the United States so you can find one close to you.Getting screened is affordable. The most popular package at Life Line Screening includes 5 screenings in 1 appointment for $149.Get the most out of your life! Find out your stroke and cardiovascular disease risk with Life Line Screening so you can be in control and do something about it.***CLICK HERE*** to schedule your appointment! A simple screening can be worth a lifetime.1 American Heart Association https://www.heart.org/en/get-involved/advocate/federal-priorities/cdc-prevention-programs2 Hackam DG, Karpral MK, et al. Most stroke patients do not get a warning, a Population Based Cohort Study. Sept. 2009. Neurology, 73, 1074-1075.